Cardiac Care
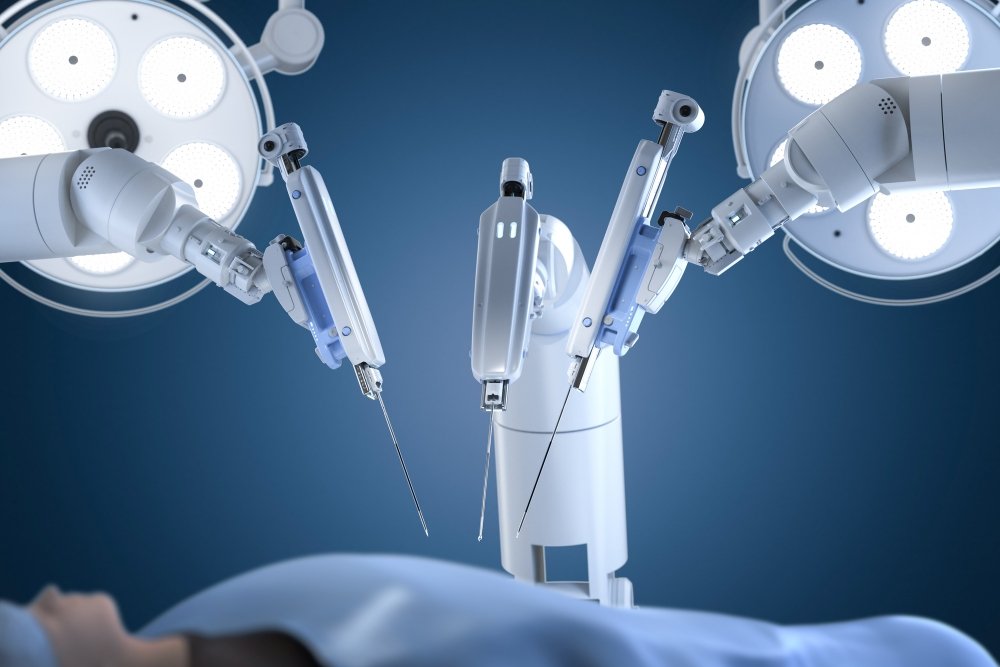
Heart surgery has long been associated with large incisions, long hospital stays, and extended recovery times. But in recent years, a quiet revolution has been changing the landscape of cardiac care. Minimally invasive heart surgery (MIHS) has emerged as a powerful, patient-friendly alternative to traditional open-heart procedures. With smaller incisions, faster recovery, and fewer complications, this modern medical marvel is reshaping how we treat heart conditions.
Let’s dive deep into how this gentle revolution is transforming lives and redefining the future of cardiac surgery.
Minimally invasive heart surgery refers to procedures performed through small incisions (often 2 to 4 inches) rather than the traditional 6 to 10-inch cut through the breastbone. The primary goal is to reduce trauma to the body while ensuring effective surgical outcomes.
The core principles include:
| Feature | Traditional Open-Heart Surgery | Minimally Invasive Heart Surgery |
| Incision | Large, full sternotomy (6–10 inches) | Small incisions (2–4 inches) |
| Recovery Time | 6–8 weeks | 2–4 weeks |
| Hospital Stay | 5–10 days | 3–5 days |
| Pain and Scarring | More discomfort, visible scars | Less pain, smaller scars |
| Risk of Infection | Higher | Lower |
The journey of minimally invasive heart surgery began in the 1990s, driven by innovations in imaging, instrument design, and robotics. Key milestones include:
With ongoing technological advances, these techniques continue to evolve and expand.
Modern MIHS heavily relies on real-time imaging such as:
These tools allow surgeons to see the heart in motion and plan their approach with confidence.
Key tools include:
These technologies allow for greater accuracy, less tissue damage, and better patient outcomes.
Not every patient is a candidate. Ideal patients:
Detailed pre-surgical imaging helps determine if the heart’s anatomy is suitable for a minimally invasive approach.
III. Types of Heart Conditions Treated with Minimally Invasive Methods
Preparation includes:
Patients are educated about what to expect before, during, and after surgery.
During surgery:
The surgeon may work directly or via a robotic interface, depending on the approach.
After surgery:
Most patients return home in 3 to 5 days and resume light activities within 2 weeks.
Patients undergoing MIHS often:
Smaller incisions mean:
While MIHS may seem costlier upfront due to tech use, it often:
Even with advanced techniques, risks include:
MIHS may not be suitable if:
Summary
Minimally invasive heart surgery is reshaping cardiac care. By minimizing trauma, reducing recovery time, and improving outcomes, it offers a gentler, more effective alternative to traditional open-heart surgery. Thanks to robotic systems, advanced imaging, and innovative techniques, procedures that once required large incisions and long recoveries can now be completed with tiny openings and shorter downtime.
As technology advances, these approaches are becoming available to more patients across the globe. While not everyone may qualify for MIHS, those who do often experience fewer complications, faster healing, and better quality of life.
Frequently Asked Questions
Q: How long does recovery take after minimally invasive heart surgery compared to traditional surgery?
A: Most patients recover within 2–4 weeks after minimally invasive surgery, versus 6–8 weeks for open-heart surgery. Pain levels are lower, and activity resumes sooner.
Q: Are all heart conditions suitable for minimally invasive surgical treatment?
A: No. Your eligibility depends on your condition’s complexity, previous surgeries, overall health, and your heart’s anatomy.
Q: Is minimally invasive heart surgery as effective as traditional open-heart surgery?
A: Yes, for selected patients. Studies show comparable outcomes with faster recovery and fewer complications.
Q: What are the main risks associated with minimally invasive heart surgery?
A: Risks include bleeding, infection, blood clots, and the possibility of switching to open surgery if needed.
Q: How do I know if I’m a candidate for minimally invasive heart surgery?
A: Your cardiac surgeon will assess your condition, imaging, and medical history to determine if MIHS is safe and effective for you.
The era of big incisions and long recoveries is being replaced by precision, safety, and speed. The gentle revolution of minimally invasive heart surgery is here – and it’s changing lives, one heartbeat at a time.